
AI in Healthcare: ROI Case Studies
Healthcare Technology
Updated Jan 19, 2026
Case studies show AI virtual assistants, coding automation, and remote monitoring deliver rapid ROI—averaging 451%—and multi-million-dollar savings for health systems.
AI is reshaping healthcare by delivering measurable financial and operational results. Key takeaways from recent case studies include:
AI Virtual Assistants: Tools like Clare and Eleanor streamline patient communication, saving costs and increasing revenue. For example, OSF HealthCare saved $1.2M in contact center costs and gained $1.2M in annual revenue.
Medical Coding and Billing: AI solutions like Nym and H2O Document AI reduce coder workloads and improve billing accuracy. Inova Health System saved $1.3M annually and cut their DNFB backlog by 50%.
Remote Patient Monitoring: Platforms like UnityPoint Health's Readmission Heat Map and Emory Healthcare's eICU reduce hospital readmissions and improve patient outcomes. UnityPoint saved $32.2M over 30 months.
With an average ROI of 451%, these AI implementations show that healthcare systems can save millions while addressing challenges like staff shortages and physician burnout. As 80% of healthcare CIOs plan major AI investments by 2026, the focus is on scaling solutions that deliver quick and measurable benefits.
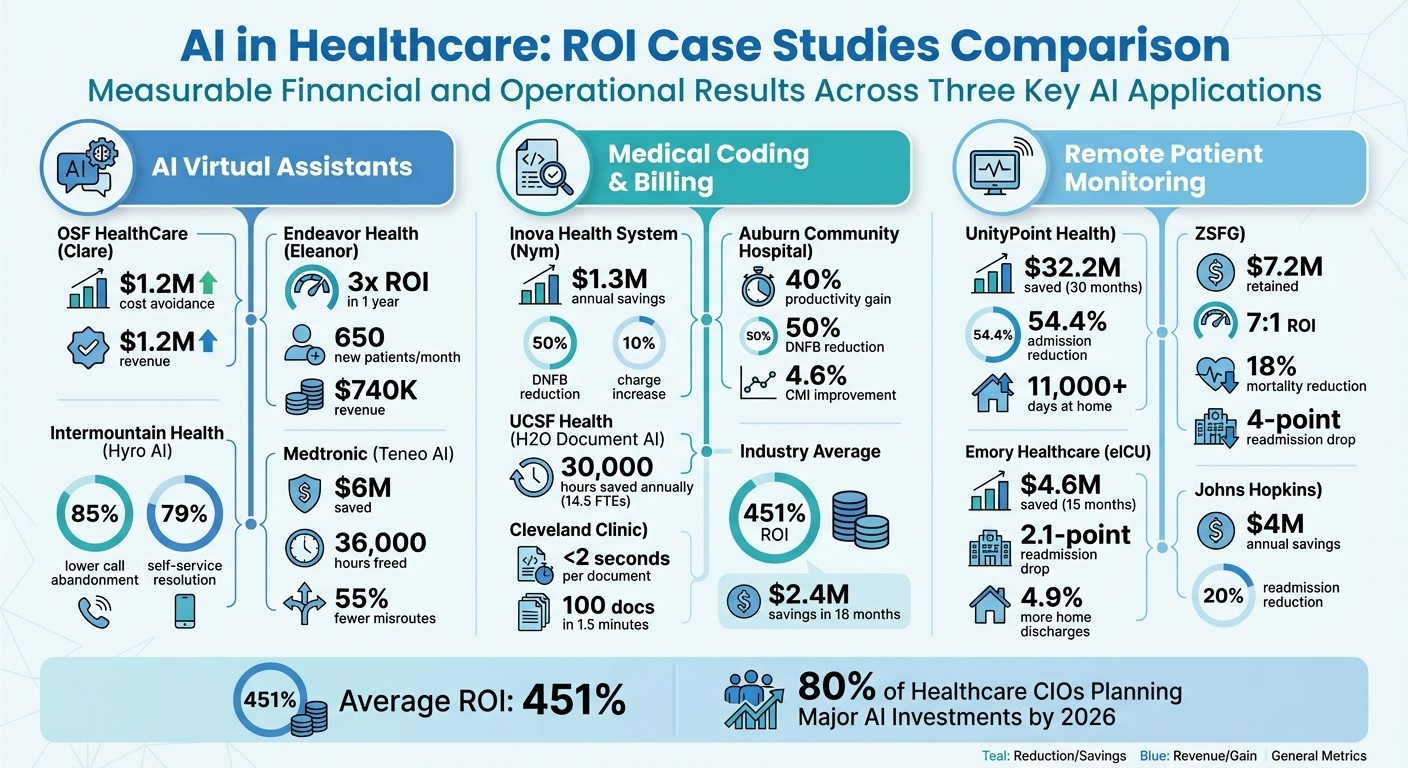
AI Healthcare ROI Comparison: Cost Savings and Results Across 3 Implementation Categories
Case Study 1: AI Virtual Assistants in Healthcare
Deployment and Key Features
AI virtual assistants are reshaping how healthcare organizations interact with patients, acting as a 24/7 digital gateway for services like symptom checking, appointment scheduling, and patient navigation. These systems seamlessly integrate with Electronic Health Record (EHR) platforms like Epic, as well as CRM and contact center software, ensuring a smooth and unified patient experience.
For example, OSF HealthCare joined forces with Fabric in 2024 to launch "Clare", an AI-powered virtual care assistant. Clare provides round-the-clock access for symptom checking and appointment scheduling, making it easier for patients to connect with care when they need it most [6]. Similarly, Endeavor Health introduced "Eleanor", a tailored AI assistant integrated into their website and patient portal. Eleanor helps patients find doctors and book same-day appointments effortlessly [8].
Intermountain Health tackled the challenge of data silos resulting from mergers by centralizing operations through robust system integrations. This move enabled them to gain a comprehensive view of the patient journey [2]. Meanwhile, Medtronic upgraded its legacy IVR systems with conversational AI, rolling it out across more than 60 contact centers. The results? A 55% reduction in misrouted calls, 37% shorter wait times, and compliance with HIPAA regulations. This overhaul saved $6 million and freed up 36,000 agent hours in 2022 [7].
Interestingly, about 27% of patient inquiries occur outside of regular business hours [2]. AI virtual assistants step in during these times, reducing missed opportunities and enhancing patient satisfaction. These integrations not only simplify patient interactions but also deliver substantial financial benefits.
Results and ROI Analysis
The impact of AI virtual assistants is evident in both cost savings and revenue growth.
OSF HealthCare reported avoiding $1.2 million in contact center costs while generating an additional $1.2 million in annual net revenue from new patients who accessed care through Clare [6]. Endeavor Health saw a threefold return on investment (ROI) within just one year of deploying Eleanor. The system brought in 650 new patients each month, contributing $740,000 in patient revenue while cutting $300,000 in contact center costs [8].
"With Hyro's Smart Routing in our call centers, we saw an improvement drop in our abandonment rates and in speed to answer. That's great performance and such a win for our patients!"
– Mona Baset, VP Digital Services, Intermountain Health [2]
Intermountain Health experienced an 85% reduction in call abandonment rates, a 79% improvement in speed to answer, and resolved 79% of patient chats without needing human intervention [2].
Medtronic's adoption of conversational AI across multiple business units achieved a 99% accuracy rate in understanding caller needs. This improvement slashed the cost per contact from $25.96 to under $12 [7].
Health System | AI Solution | Key Outcome | Financial Impact |
|---|---|---|---|
OSF HealthCare | Clare (Fabric) | 24/7 Access | $1.2M Cost Avoidance + $1.2M Revenue [6] |
Endeavor Health | Eleanor (Fabric) | 650 New Patients/Month | 3x ROI in 1 Year [8] |
Intermountain Health | Hyro AI | 85% Lower Abandonment | 79% Self-Service Resolution [2] |
Medtronic | Teneo AI | 55% Fewer Misroutes | $6M Saved, 36K Hours [7] |
"With Teneo, we achieved better results than we could have imagined, and the success in Cardiovascular led other contact centers to adopt the same approach."
– Michael Altieri, Service Delivery Manager, Virtual Assistants, Medtronic [7]
These examples highlight how AI virtual assistants not only streamline operations but also deliver tangible financial results. Many organizations see a return on their investment within the first year, proving the value of these advanced tools in modern healthcare.
Case Study 2: AI for Medical Coding and Billing
Implementation Details
Medical coding and billing have become major hurdles for healthcare organizations. Challenges like staff shortages, increasing patient numbers, and the high cost of contract coders have driven many systems to adopt AI-powered solutions. These tools use technologies like Intelligent Character Recognition (ICR) and Natural Language Processing (NLP) to extract data from clinical documents and input billing codes into Electronic Health Record (EHR) systems.
Take Inova Health System in Northern Virginia, for example. With their Emergency Department facing overwhelming patient volumes and coder shortages, they were forced to implement mandatory overtime, which only worsened their discharged-not-final-billed (DNFB) backlog. In 2026, they introduced Nym's autonomous medical coding engine for facility coding in their emergency departments across multiple hospitals. This system integrates directly with their existing EHR, processes charts independently, and ensures full compliance with HIPAA regulations [9].
Typically, investing in Revenue Cycle AI costs between $100,000 and $300,000, with payback periods ranging from 8 to 14 months [1]. Meanwhile, UCSF Health opted for a different approach. They implemented H2O Document AI to handle their 1.4 million annual e-faxes, which include referrals, billing details, and prescription refills. Their "Intake Automation" system classifies and extracts data from semi-structured documents, eliminating hours of manual work [5].
"When we started this journey, we were hopeful that information extraction from semi-structured documents was possible, but we weren't sure... Now that the UCSF-H2O.ai collaboration team has delivered, it opens up many possibilities."
– Bob Rogers, PhD, Expert in Residence for AI, UCSF [5]
Another notable example is Cleveland Clinic, which adopted autonomous coding technology capable of reading each document in under 2 seconds and processing over 100 documents in just 1.5 minutes. This dramatically accelerated their billing cycle [1].
These examples highlight how AI solutions are transforming medical coding, delivering both operational efficiency and financial benefits.
Efficiency Gains and ROI
The financial and operational impact of AI coding systems is hard to ignore. Inova Health System, for instance, saved $1.3 million annually on coding costs, eliminated mandatory overtime for their coding staff, and reduced their DNFB backlog by 50%. Additionally, they experienced a 10% increase in average charges per ED encounter due to improved charge capture, ensuring all services were billed accurately [9].
Auburn Community Hospital saw a 40% boost in coder productivity and halved their DNFB cases. They also improved their case mix index by 4.6%, reflecting more precise coding of patient complexity [1]. At UCSF Health, their automation initiative is expected to save 25,000 hours of staff time and 5,000 hours of clinician time annually - equivalent to about 14.5 full-time employees [5].
Industry-wide, Revenue Cycle AI has proven to deliver a 40%+ increase in coder productivity and reduce claims review time by up to 63% [1]. On average, healthcare facilities report an ROI of 451%, with mid-sized organizations saving around $2.4 million within 18 months of implementing these systems [1].
Here’s a quick comparison of outcomes from different health systems:
Health System | AI Solution | Key Outcome | Financial Impact |
|---|---|---|---|
Inova Health System | Nym Autonomous Coding | 50% DNFB Reduction | $1.3M Annual Savings [9] |
Auburn Community Hospital | Revenue Cycle AI | 40% Productivity Gain | 50% DNFB Reduction [1] |
UCSF Health | H2O Document AI | 1.4M Faxes Automated | 30,000 Hours Saved [5] |
Cleveland Clinic | Autonomous Coding | 100 Docs in 1.5 Min | <2 Sec Per Document [1] |
These results underscore the transformative potential of AI in healthcare operations. Beyond just cutting costs, these systems free up coders to focus on more complex tasks like insurance advocacy and detailed reviews, rather than routine data entry.
Case Study 3: AI Remote Patient Monitoring
System Setup and Costs
AI-driven remote patient monitoring systems are transforming healthcare by reducing readmissions and improving outcomes. These systems analyze a wide range of patient data - lab results, social factors, and historical patterns - to predict which patients are at risk of complications after discharge. By integrating with electronic health records (EHRs), they provide a detailed risk profile for each patient.
UnityPoint Health adopted the Health Catalyst Data Operating System along with the "Readmission Heat Map" AI tool to manage patients with chronic conditions. This tool offers a visual dashboard that helps care managers quickly identify patients in need of immediate attention, tracking metrics like missed appointments and recent hospitalizations [11].
Similarly, ZSFG implemented the Epic Risk of Unplanned Readmission V2 model for heart failure patients, investing $1 million in the process [10]. Industry data shows that setting up predictive AI systems for readmissions typically costs between $75,000 and $200,000, with payback periods ranging from 12 to 18 months [1]. Meanwhile, Emory Healthcare deployed the Philips eICU platform across 136 beds at five hospital locations, enabling remote monitoring of critically ill patients [12].
These upfront investments pave the way for both operational improvements and significant financial returns.
Outcomes and Financial Impact
The results speak volumes about the potential of AI in healthcare. These examples highlight how targeted AI investments can lead to cost savings and better patient care.
UnityPoint Health saw impressive results, saving $32.2 million over 30 months. Their program achieved a 54.4% reduction in hospital admissions and a 39% drop in emergency department visits, while patients enjoyed over 11,000 additional days at home rather than in the hospital [11].
"Our successful partnerships leverage the strengths of clinicians and analysts. The team was empowered to build and enhance analytic tools that support the most vulnerable patients, reducing unnecessary utilization and decreasing healthcare spending by more than $32M."
– Rhiannon Harms, Executive Director Strategic Analytics, UnityPoint Health [11]
At ZSFG, heart failure readmissions dropped by 4 percentage points - from 27.9% to 23.9% - resulting in $7.2 million retained through pay-for-performance funds and a 7:1 ROI on their $1 million investment. Additionally, they achieved an 18% reduction in all-cause mortality for heart failure patients [10].
An independent audit by Abt Associates for CMS revealed that Emory Healthcare's eICU platform reduced Medicare spending by $1,486 per 60-day episode, totaling $4.6 million in savings over 15 months. The program also led to a 2.1 percentage point drop in 60-day inpatient readmissions and a 4.9% increase in patients discharged directly home [12].
Health System | AI Solution | Key Outcome | Financial Impact |
|---|---|---|---|
UnityPoint Health | Readmission Heat Map | 54.4% Admission Reduction | $32.2M Savings (30 mos) [11] |
ZSFG | Epic Readmission Risk V2 | 4-Point Readmission Drop | $7.2M Retained (7:1 ROI) [10] |
Emory Healthcare | Philips eICU Platform | 2.1-Point Readmission Drop | $4.6M Savings (15 mos) [12] |
Predictive Risk Models | 20% Readmission Reduction | $4M Annual Savings [1] |
Johns Hopkins Hospital used predictive risk models to analyze diagnosis codes, lab results, and social factors, identifying high-risk patients. This approach led to a 20% reduction in 30-day readmissions and generated $4 million in annual savings [1].
"These independent findings verify that our innovative approach to addressing a highly variable, complex patient population – those in the critical care unit – improves patient outcomes, allowing them to leave the ICU healthier, thereby reducing the need for patients and their families to have extended rehab stays or be readmitted."
– Dr. Timothy Buchman, Director, Critical Care Center, Emory Healthcare [12]
These case studies clearly show how AI-powered remote monitoring not only cuts costs but also revolutionizes care for vulnerable patients by improving outcomes and reducing unnecessary hospital stays.
How a Major Healthcare Provider Saved 500,000 Hours With AI Agents | StackAI
Lead Receipt: AI Receptionists and Workflow Automation
Lead Receipt is making waves in healthcare with AI-driven solutions that deliver measurable returns for medical practices.
Key Features and Benefits
Lead Receipt offers 24/7 AI receptionists and workflow automation, ensuring no potential patient slips through the cracks - even during the 27% of inquiries that come in after regular business hours [2]. With this system, missed calls and delayed responses become a thing of the past.
The platform seamlessly integrates with existing EHR and CRM systems, like Salesforce, allowing for real-time appointment booking and automatic data entry - all without disrupting current workflows [13][14]. By automating repetitive tasks like appointment confirmations, cancellations, and benefits verification, healthcare staff can focus on what matters most: addressing complex patient needs [5][14]. Plus, its multilingual capabilities make it accessible to diverse patient populations, while its analytics provide actionable insights to improve patient engagement and streamline daily operations.
These features collectively help healthcare practices operate more efficiently and effectively.
ROI Potential with Lead Receipt
Lead Receipt's pricing plans are designed to fit various needs and budgets:
Starter Plan: $300/month, offering 24/7 web-chat services.
Professional Plan: $750/month, providing voice and chat services for up to 100 AI calls daily in five languages.
Enterprise Plan: Custom pricing with unlimited calls and dedicated AI consulting.
The financial benefits speak for themselves. On average, healthcare organizations using AI receptionists and workflow automation report $2.4 million in savings for mid-sized facilities within 18 months [1]. By capturing after-hours inquiries and reducing call abandonment, practices can prevent revenue loss and cut down on administrative expenses. Additionally, AI-powered scheduling slashes appointment booking times from three days to just 28 minutes [15], significantly boosting patient satisfaction and staff efficiency. This kind of round-the-clock responsiveness doesn’t just save time - it converts leads into loyal patients.
Key Takeaways from AI ROI Case Studies
The case studies highlighted above reveal several key strategies behind successful AI adoption in healthcare.
Healthcare organizations that saw the best returns shared three major factors: early investment, tailored solutions, and integrated workflows. For example, HonorHealth saved an impressive $62 million by starting its AI journey early in 2021, giving them ample time to refine processes while others were still in the pilot phase [4]. Similarly, UC Davis Health developed a custom predictive model that surpassed commercially available options. Dr. Reshma Gupta noted, "Our internally developed AI model outperforms a number of other out-of-the-box AI models purchased externally" [15].
For organizations just beginning their AI journey, ambient documentation offers a promising starting point. This method boasts quick payback periods - typically 6 to 12 months - with implementation costs ranging from $50,000 to $150,000 [1]. Beyond financial benefits, it also addresses physician burnout by cutting down after-hours documentation and improving staff morale [15][5]. A 90-day pilot at Seattle Children's with Abridge ambient AI showed impressive results: a 15.5% reduction in time spent on notes per visit and a 77% drop in overall charting effort [3].
AI doesn't just enhance existing workflows; it often replaces outdated processes entirely. As Kathi Zarubi, Chief Nursing Officer at HonorHealth, explained, "Implementing AI solutions is not like implementing a typical technology upgrade. AI solutions create new workflows and eliminate others" [4]. Success in this area requires strong clinical leadership and a willingness to rethink daily routines. Establishing AI labs or Centers of Excellence can help test ideas, validate use cases, and avoid costly mistakes before scaling across the organization [3][15]. These operational insights are essential for understanding the broader financial impacts of AI adoption.
Data shows that many healthcare organizations achieve ROI within the first year, with measurable savings across various operational areas [1].
Finally, investing in your team is just as important as investing in technology. Upskilling programs and AI Learning Academies can accelerate adoption and ensure better use of AI tools [3]. Donna Roach, Chief Digital and Information Officer at University of Utah Health, summed it up perfectly: "The greatest return this year has been clarity - knowing what works, what doesn't, and how to scale AI safely within a complex health system" [3]. This highlights how human expertise and technological advancements must go hand in hand for long-term success.
Conclusion
Case studies highlight how AI can lead to impressive financial outcomes. Take HonorHealth, for instance - they managed to save $62 million, while Northeast OB/GYN slashed their operational costs by 40% [4][14].
But the financial wins are just part of the story. A complete overhaul of workflows has proven just as important. As Kathi Zarubi from HonorHealth explained:
"Implementing AI solutions is not like implementing a typical technology upgrade. AI solutions create new workflows and eliminate others" [4].
This shift helps streamline operations, cutting out repetitive manual tasks so healthcare professionals can focus on more meaningful, high-impact work.
Front-desk automation is another area where AI delivers quick returns. Tools like Lead Receipt act as 24/7 virtual receptionists, handling patient inquiries, scheduling, and lead management. These solutions ensure no interaction is missed, even outside regular office hours [2]. Such advancements highlight the broader potential of AI in transforming healthcare operations.
With 80% of healthcare CIOs planning to make major AI investments by 2026 [1], adopting AI is no longer optional - it’s becoming essential. Whether the goal is easing physician burnout, improving patient flow, or increasing revenue, AI tools like Lead Receipt provide a reliable and effective way forward.
FAQs
How can AI virtual assistants enhance patient communication and lower healthcare costs?
AI virtual assistants are transforming patient communication by offering round-the-clock support for tasks like symptom checks, scheduling appointments (whether in-person, virtual, or asynchronous), and providing triage guidance. Thanks to natural language understanding, these assistants allow patients to communicate naturally, ensuring they receive accurate, timely information and are quickly directed to the right resources.
By handling routine inquiries and appointment scheduling, healthcare systems can significantly cut staffing and call center costs. For instance, one health system reported saving over $1.2 million in contact center expenses while generating an additional $1.2 million in new patient revenue in just one year. Similarly, another organization achieved a 40% reduction in operational costs and resolved half of all inbound calls without requiring human intervention. These examples highlight how AI solutions not only improve patient access and satisfaction but also deliver impressive financial returns.
What are the financial benefits of using AI for medical coding and billing?
AI-powered medical coding and billing systems are transforming how U.S. healthcare providers manage their finances, delivering impressive cost savings and revenue growth. In fact, many organizations report an average ROI of 451% and savings of $2.4 million within just 18 months of adopting these systems. Some hospitals have saved as much as $4 million by automating their documentation and coding workflows.
These tools are game-changers when it comes to reducing labor costs, speeding up claim submissions, and improving coding accuracy. Fewer errors mean fewer claim denials and faster reimbursements. For example, one health system slashed annual coding costs by $1.3 million, boosted charge capture by 10%, and cut denied and unbilled claims in half. Another provider reported a 64% reduction in manual coding, trimmed coding delays by 3.6 days, and automated 71% of their processes, resulting in faster cash flow and fewer mistakes.
By enhancing efficiency and accuracy, AI in medical coding and billing not only simplifies operations but also delivers measurable financial results for healthcare providers.
How does AI-powered remote patient monitoring improve care and prevent hospital readmissions?
AI-powered remote patient monitoring (RPM) leverages data from wearables, home sensors, and connected devices to keep track of vital signs and activity patterns in real time. By using machine learning, it identifies potential red flags - like elevated blood pressure, irregular heart rhythms, or low oxygen levels - and notifies healthcare teams to take swift action. This might involve adjusting medications or scheduling a telehealth visit.
This forward-thinking approach is especially helpful for managing chronic conditions. It keeps patients stable at home and cuts down on emergency care. Research shows that AI-driven RPM can reduce hospital admissions for chronic-disease patients by as much as 40%, slashing costs and improving health outcomes. It’s also proven effective in lowering 30-day readmission rates by spotting high-risk patients early and ensuring they get timely follow-up care.
